Lateral hip pain and the peri-menopausal woman
One of the facts of being female and aged between 45 and 55 years old is that you are most likely in the peri-menopausal window of your life.
And the research tells us that 1 in 4 peri-menopausal will suffer with lateral hip pain.
Why is this?
We all know the common symptoms of menopause including hot flushes, sleep disturbances, mood changes and weight gain but the lowering of our oestrogen also affects the musculoskeletal system.
One of the facts of being female and aged between 45 and 55 years old is that you are most likely in the peri-menopausal window of your life.
And the research tells us that 1 in 4 peri-menopausal will suffer with lateral hip pain.
Why is this?
We all know the common symptoms of menopause including hot flushes, sleep disturbances, mood changes and weight gain but the lowering of our oestrogen also affects the musculoskeletal system.
It does this by reducing our collagen production. Bone can be affected which means menopausal women might have issues with decreased bone density or osteoporosis. Less collagen production also can lead to sarcopenia which is a loss of muscle mass.
But what I want too talk about today is the peri-menopausal lower oestrogen levels and it’s effect on collagen production and tendon health.
Menopausal women’s tendon can be less resilient than they once were which is why seemingly mundane events can lead to tendon injury. The reduced oestrogen level is associated with a reduction in tensile strength of the tendon, less collagen synthesis, and increased degradation of tendon tissue. Oh the joy!!
I so often see the peri-menopausal women in the clinic who wakes up one morning and realises that she is suddenly 10 kgs heavier than she once was so decides to embark on a get fit quick program. Next thing she starts experiencing tendon pain. Sometimes it’s the Achilles Tendon, other times it’s the knee or patella tendon or sometimes the lateral hip or gluteal tendon that becomes problematic.
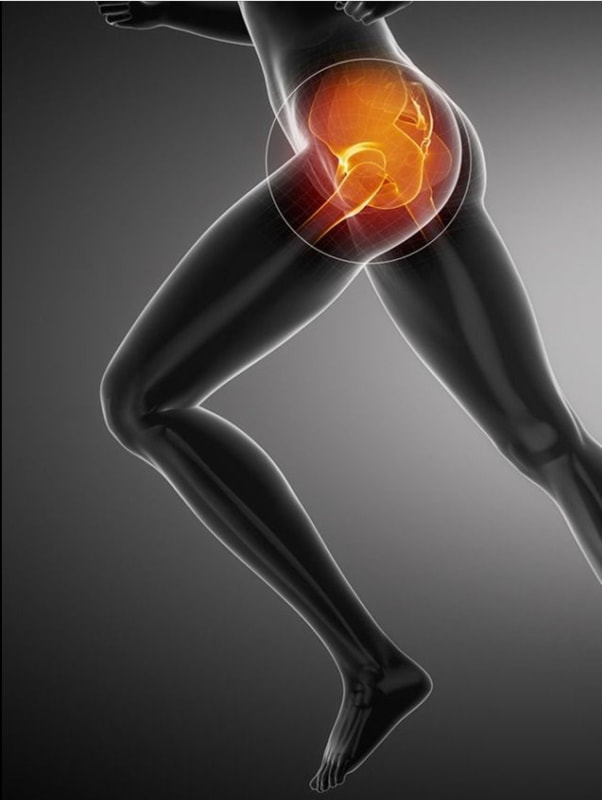
Let’s talk about the hip.
The lateral hip pain can be excruciating, often women will report being unable to sleep on the affected hip and will have intense pain when climbing stairs. In severe cases she might even have trouble standing on one leg to get dressed
In the old days it was called Trochanteric Burisits and treatment was aimed at reducing the ‘inflammation’ often by icing, anti-inflammatories , ‘stretching’ the ITB and maybe even cortisone injections if the symptoms didn’t resolve.
We now know that 90% of lateral hip pain is actually caused by what is known as gluteal tendinopathy.
Tendons can be finicky. The don’t like changes in oestrogen levels, they don’t like changes in load, they don’t like compression and they don’t like being stretched.
Symptoms of gluteal tendinopathy are
How we manage gluteal tendinopathy
The keys to managing this lateral hip pain are to
1. Walking
Sometimes in their enthusiasm to get the menopausal weight off women will start walking Castle hill, striding out which puts a sudden increase of load on the gluteal tendon. So the key is to avoid over striding. Also there can be foot related internal rotation of the thigh during gait which can increase the compression of the tendon at the lateral hip
2. Standing
It’s tempting sometimes when the hip is sore to ‘hang’ off the hip but this can increase compression of the tendon. Try to stand evenly
3. Sitting
Believe it or not, sitting with your legs crossed can increase the compression of the gluteal tendon on the bone. So sit with both feet firmly planted on the ground
4. Sleeping
Using an eggshell foam topper is a great way to reduce compression of the lateral hip when sleeping on the affected hip and using a pillow between the knees can prevent the stretching of the tendon on the top leg.
5. Avoid stretching
As previously mentioned, tendons don’t like being stretched Especially avoid ITB stretches, glute stretches that include flexion and adduction of the hip
6. Get strong
Clam exercises can actually increase compression of the gluteal tendon so avoid those but definitely the best way to improve your pain is to get those glutes strong. A progressive strength program is key! Think gluteal bridges, single leg standing, squats etc...
Yes, there other conditions that cause lateral hip pain, so as always, if in doubt get it checked out
But in most cases we can settle your lateral hip pain by looking at the way you walk, the way you stand, the way you sit, improving your sleeping position and getting you strong again
Further reading
Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. Vincenzio B et al BMJ, May 2018
Gluteal Tendinopathy: Integrating Pathomechanics and Clinical Features in its Management. Grimaldi A. Joournal of Orthopedic and Sports Physical Therapy, Nov 2015
But what I want too talk about today is the peri-menopausal lower oestrogen levels and it’s effect on collagen production and tendon health.
Menopausal women’s tendon can be less resilient than they once were which is why seemingly mundane events can lead to tendon injury. The reduced oestrogen level is associated with a reduction in tensile strength of the tendon, less collagen synthesis, and increased degradation of tendon tissue. Oh the joy!!
I so often see the peri-menopausal women in the clinic who wakes up one morning and realises that she is suddenly 10 kgs heavier than she once was so decides to embark on a get fit quick program. Next thing she starts experiencing tendon pain. Sometimes it’s the Achilles Tendon, other times it’s the knee or patella tendon or sometimes the lateral hip or gluteal tendon that becomes problematic.
Let’s talk about the hip.
The lateral hip pain can be excruciating, often women will report being unable to sleep on the affected hip and will have intense pain when climbing stairs. In severe cases she might even have trouble standing on one leg to get dressed
In the old days it was called Trochanteric Burisits and treatment was aimed at reducing the ‘inflammation’ often by icing, anti-inflammatories , ‘stretching’ the ITB and maybe even cortisone injections if the symptoms didn’t resolve.
We now know that 90% of lateral hip pain is actually caused by what is known as gluteal tendinopathy.
Tendons can be finicky. The don’t like changes in oestrogen levels, they don’t like changes in load, they don’t like compression and they don’t like being stretched.
Symptoms of gluteal tendinopathy are
- Pain over the outside of the hip at the level of the greater trochanter
- Pain when sleeping on the affected hip
- Pain sleeping with the affected hip on top. This happens because as the hip adducts or crosses over the midline it puts a stretch on the gluteal tendon.
- Difficulty, and it can be very painful, to walk up stairs
How we manage gluteal tendinopathy
The keys to managing this lateral hip pain are to
1. Walking
Sometimes in their enthusiasm to get the menopausal weight off women will start walking Castle hill, striding out which puts a sudden increase of load on the gluteal tendon. So the key is to avoid over striding. Also there can be foot related internal rotation of the thigh during gait which can increase the compression of the tendon at the lateral hip
2. Standing
It’s tempting sometimes when the hip is sore to ‘hang’ off the hip but this can increase compression of the tendon. Try to stand evenly
3. Sitting
Believe it or not, sitting with your legs crossed can increase the compression of the gluteal tendon on the bone. So sit with both feet firmly planted on the ground
4. Sleeping
Using an eggshell foam topper is a great way to reduce compression of the lateral hip when sleeping on the affected hip and using a pillow between the knees can prevent the stretching of the tendon on the top leg.
5. Avoid stretching
As previously mentioned, tendons don’t like being stretched Especially avoid ITB stretches, glute stretches that include flexion and adduction of the hip
6. Get strong
Clam exercises can actually increase compression of the gluteal tendon so avoid those but definitely the best way to improve your pain is to get those glutes strong. A progressive strength program is key! Think gluteal bridges, single leg standing, squats etc...
Yes, there other conditions that cause lateral hip pain, so as always, if in doubt get it checked out
But in most cases we can settle your lateral hip pain by looking at the way you walk, the way you stand, the way you sit, improving your sleeping position and getting you strong again
Further reading
Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. Vincenzio B et al BMJ, May 2018
Gluteal Tendinopathy: Integrating Pathomechanics and Clinical Features in its Management. Grimaldi A. Joournal of Orthopedic and Sports Physical Therapy, Nov 2015